Skin and Skin Structure Infections
- Skin and skin-structure infections (SSSIs) are infections of the epidermis, dermis or subcutaneous tissue
- SSSI are common presentations in bacterial diseases → most common are S. aureus and S. pyogenes (Group A)
I. Integumentary System Review:
- the skin (integument) is the largest body organ and functions to:
- protect against injury (e.g., toxins, mechanical insults, UV radiation)
- regulate body temperature
- maintain fluid balance (i.e., protect against dehydration)
- serve as sensory organ
- immune system surveillance against potential threats
- synthesize vitamin D3 (cholecalciferol)
- the skin is also dynamic in a constant state as the cells making up the outer surface (epidermidis) are continuously being shed and replaced by underlying cells arising from the dermis layer
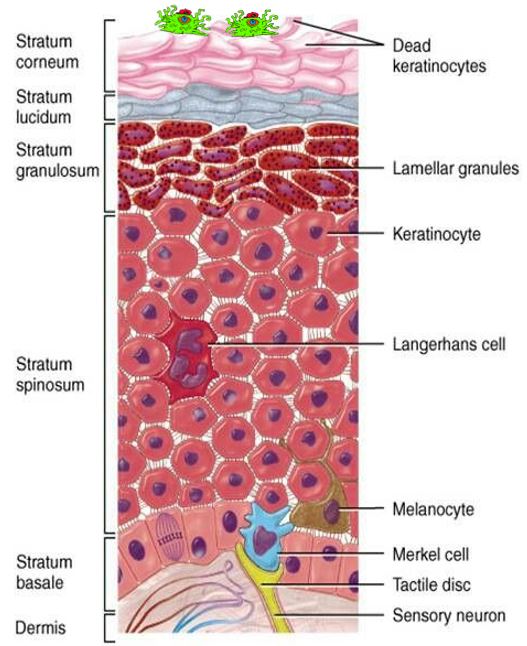
(a) Epidermidis
- epidermis is striated squamous epithelium comprised of keratinocytes, which synthesize the fibrous structural protein keratin
(b) Dermoepidermal junction
- i.e., basement membrane joining the epidermidis and dermis layer
- basal layer cells are connected via adhesion proteins (desmosomes) and intracellular keratin cytoskeleton
II. Infections of the Integumentary System
- referred to as skin and skin tissue/structure infections (SSTI/SSSI), now more often called acute bacterial skin and skin structure infections (ABSSSI) → distinguish between bacteria, fungal, and viral SSSIs
- uncomplicated SSSI (uSSSI/uABSSSI): localized and confined to the epidermis and dermis layers
- e.g., impetigo, folliculitis, furuncles, erysipelas, superficial abscesses, wound infections, uncomplicated cellulitis
- generally caused by S. aureus and S. pyogenes (Group A) → commensal bacteria
- complicated SSSI (cSSSI/cABSSSI): infection of deeper skin structures (e.g., fascia, muscle) that requires surgical intervention or occurs in the presence comorbidities (e.g., HIV, diabetes mellitus)
- e.g., complicated cellulitis, necrotizing fasciitis, myositis, gas gangrene, major abscesses, infected burns and ulcers, infected bite wounds, diabetic foot infections
II. Infections of the Integumentary System
(a) Dermatologic (confined to epidermis and dermis)
- impetigo – S. aureus* (* most common), S. pyogenes
- folliculitis – S. aureus*, P. aeruginosa, P. acnes
- carbuncle, furuncle – S. aureus* including CA-MRSA
- vesicles – viruses only
- nodules – viruses only
- uncomplicated abscess – S. aureus* including CA-MRSA, other commensal skin bacteria
- granulomas – Mycobacterium marinum, M. tuberculosis, Mycobacterium leprae
- uncomplicated cellulitis – β-hemolytic streptococci (groups A, B, C, G F) > S. aureus >> H. influenzae b, V. vulnificus, C. perfringens, B. anthracis, Enterobacteriaceae, P. aeruginosa
- erysipelas – S. pyogenes (group A strep)*, Vibrio vulnificus, Aeromonas hydrophila
(b) Soft Tissue (subcutaneous tissues, connective tissues, fascia)
- complicated cellulitis – S. pyogenes*
- complicated abscess – S. aureus*
- erysipelas – S. pyogenes*
- necrotizing fasciitis – S. pyogenes, anaerobes (Clostridium, Bacteriodes, Peptostreptococcus), Vibrio
- lymphadenitis – Brucella, M. avium-intracellulare, M. tuberculosis, B. henselae, S. pyogenes, T. pallidum
- infected bites – Eikenella, Pasteurella, oral anaerobes (Peptostreptococcus, Fusobacterium, Prevotella, Porphyromonas) staphylococci, streptococci, Haemophilus
- infected burns – Staph/Strep, P. aeruginosa, Enterobacteriaceae
- gas gangrene – C. perfringens, anaerobes
- pyomyositis – S. aureus* including MRSA
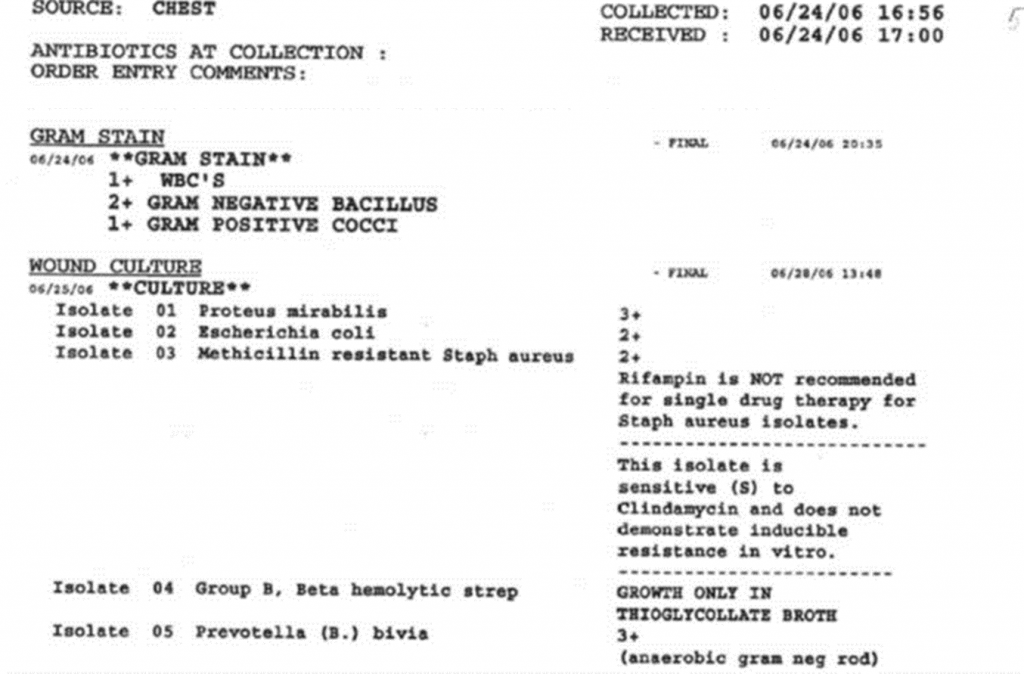
(c) Clinical Microbiology of SSSIs
- specimens are obtained from exogenous or endogenous wound or abscess sites suspected of infection
- specimens obtained by swab, removal of purulent material (e.g., pus), or needle aspiration
- in clinical microbiology reports, cell counts are semi-quantified → 1+ = cells rare in number; 2+ = moderate; 3+ = many; 4+ = great many
- wound infections are usually polymicrobial
III. Superficial Skin Infections (Uncomplicated)
- uSSSIs that are localized (non-systemic) infections of the epidermidis and dermis
- pathophysiology: bacteria invade through a break in skin (e.g., trauma, insect bite, cutaneous disease); colonizes local tissue (e.g., folliculitis, local abscess) or spreads at the site of inoculation (e.g., erysipelas, cellulitis)
(a) Impetigo
- superficial vesiculopustular skin infection causing crust-like lesions of the face and extremities
- epidemiology: 10-20 cases per 1000 pts-yr; most common in children, elderly, and areas with poor sanitation
- signs/symptoms: red sores w/ pus that may rupture and cause crusty skin; fevers, chills, malaise
- risk factors: poverty, crowding, poor hygiene; occurs usually in warm humid conditions
- pathogens: established by skin trauma (e.g., insect bite)
- impetigo contagiosa is caused by S. pyogenes; most common in children; contagious disease
- bullous impetigo (purulent) is cause by S. aureus* due to exfoliatin release


(b) Folliculitis
- superficial infection of hair follicles that have been damaged (e.g., shaving) or blocked (e.g., sweat, makeup).
- signs/symptoms: rash, itching, pimples/pustules
- pathogens – S. aureus*, P. aeruginosa (under chlorinated hot tubs), Propionibacterium acnes (acne vulgaris)
(c) Furunculosis (boils), Carbunculosis (cluster of boils)
- furuncles (boils) are singular swollen skin infection of hair follicle; often complication of folliculitis
- carbuncles are clusters of highly swollen follicular masses.
- signs/symptoms: redden nodule initial (furuncle), no fever; swollen, deep, painful follicular mass; fever, chills, and malaise due to bacteremia common for carbuncles
- usually occurs on back of neck, face, armpit, and buttocks
- S. aureus most common pathogen; CA-MRSA causes “spider bite-like” lesions with necrotic centers
(d) Skin Abscess
- abscesses are collections of pus within the dermis and deeper skin tissues; often occurs after boil develops or skin trauma that seeds the infection
- common SSSI in IV drug users (watch for MRSA).
- characterized by localized accumulation of neutrophils in response to tissue necrosis; large bacteria numbers (e.g., 4+) are observed in purulent remove for lab diagnostics
- pathogens: S. aureus (MRSA) but, other microflora species may be involved
- signs/symptoms: fevers, chills, swelling, harden tissue (induration), redness, fluid drainage
(e) Cellulitis
- cellulitis is an acute inflammation of connective tissue
- can manifest in both the dermis and subcutaneous layer
- most common of the ABSSSI hospitalizations
- epidemiology: ~20 cases per 1000 pts-yr.; most common in elderly pts; 40-70% of cases in lower limbs
- risk factors: disruption of cutaneous barrier, lymphedema, local venous stasis, chronic edema, obesity, previous episodes
- pathogens: β-hemolytic streptococci (groups A, B, C, G F) > S. aureus >> H. influenzae b, V. vulnificus, C. perfringens, B. anthracis, Erysipelothrix, Enterobacteriaceae, P. aeruginosa
- predisposing factors: spider bites, blisters, tattoos, dry skin, eczema, animal bite, surgery, IV drug users, pregnancy, diabetes/obesity (affect blood circulation → hinder innate neutrophil immunity)
- signs/symptoms: swelling, tenderness, warmth and/or redness (erythema) of infected area; fever, chills, malaise
- cellulitis causes 25-30K deaths in the U.S. each year, many are elderly or immunocompromised
- microbiology: identifying the pathogen is uncommon for uncomplicated cellulitis
(f) Erysipelas (St. Anthony’s fire)
- cellulitis of skin involving blockage of skin and dermal lymphatics; 80% of cases in lower limbs
- can manifest in both the dermis and subcutaneous layer
- epidemiology: 0.1-2.0 cases per 1000 pts-year; most common in elderly persons; female predominance
- pathogen: S. pyogenes (GAS)
- signs/symptoms: bright red painful lesions, burning pain, raised borders, flu-like symptoms
- epidemiology: infants, young children, elderly, patients with nephrotic syndrome
- microbiology: specimen obtained by aspiration of lesion
IV. Soft Tissue/Skin Structure
(a) Infected bites
- cellulitis and deep SSTI can occur after animal or human bite.
- infection often polymicrobial involving mouth microflora bacteria
- bite wound associated pathogens:
- humans – Eikenella, oral anaerobes (Peptostreptococcus, Fusobacterium, Prevotella, Porphyromonas) staphylococci, streptococci, Haemophilus
- cats/dogs – Pasteurella multocida, Capnocytophaga canimorsus, oral anaerobes (Fusobacterium, Bacteriodes, Prevotella, Propionibacterium, Peptostreptococcus, Porphyromonas), staphylococci, streptococci
- insects/spiders – S. aureus, S. pyogenes
- signs/symptoms: pain and cellulitis at site of bite; swelling, purulent discharge
(b) Necrotizing Fasciitis
- infection that causes progressing destruction of fascia and overlying fat
- predisposing factors: trauma, surgical procedure, burns, exposure to case, Varicella, injection drug use, child birth
- signs/symptoms: fever, cellulitis, sever systemic toxicity, rapid spread infection, skin necrosis with blistering, bullae, tense edema, and/or black-blue discoloration
- “flesh-eating” pathogens – S. pyogenes (GAS)*, anaerobes, V. vulnificus, E. coli, A. hydrophila, Porphyromonas.
- many infections are polymicrobial involving aerobic-anaerobic bacteria (e.g., Clostridia + coliforms)
- Vibrio vulnificus and Aeromonas hydrophila usually waterborne infections due to traumatic wound injury (fish hook, fin stab) and preexisting open wounds, particularly in immunocompromised persons.
(c) Burn Wound Infections
- burns are skin damage caused by chemicals, electricity, heat, sunlight or radiation
- three types of burns:
- first-degree = skin damage confined to epidermis
- second-degree = epidermidis + dermis
- third-degree = epidermidis + dermis + underlying tissues
- the skin is a part of innate immunity and contains macrophages to intercept invading pathogen
- loss of the skin barrier allows microbes to feast on expose dermal tissue and potentially enter the blood stream
- species often involved in burn wound infections are Staph/Strep and P. aeruginosa (Silver sulfadiazine/Silvadene covers)
(d) Diabetic Foot Infections (DFI)
- diabetes patients have a high rate foot infection due:
- loss of pain sensation (neuropathy)
- reduced blood circulation (ischemia)
- decrease neutrophil immunity and
- weakened tissues
- due to the neuropathy and weakened tissue, the feet (usually on plantar surface) are more susceptible to trauma and open wounds may go unnoticed if pain is not felt
- opportunistic bacteria can colonize the open wounds and the infection may advance to a serious disease (e.g., osteomyelitis) before recognition by the patient
- signs/symptoms: non-healing ulcers, edema, pus, foul-smelling odor (fermenting anaerobes present), cellulitis, abscess
- clinical microbiology: necrotic tissue is removed; swab/scrape base of the ulcer/lesion or aspirate pus; specimen evaluated by Gram-stained smear and cultured under aerobic/anaerobic conditions.
- pathogens – polymicrobial, Gram-positive cocci: S. aureus, S. agalactiae, and S. pyogenes implicated most often in mild DFI.
- moderate infection – ibid plus Gram (-) aerobes (e.g., E. coli, Proteus spp., Klebsiella spp.)
- extensive and systemic – ibid plus anaerobes (Bacteriodes, Clostridium, Peptostreptococcus spp.)
- epidemiology: 55K diabetes patients per year will have lower extremities amputated due in part to unsuccessful antibiotic therapy
(e) Pressure Sores
- occurs most often in elderly, bedridden, and immobilized persons. Pressure sores (bedsores) occur in any location of body receiving inadequate oxygenated blood supply (ischemia). The ischemia (lack of oxygen) leads to tissue damage and necrosis
- wounds can be infected by skin flora bacteria (Gram-positive cocci).

